Definition:
Lesions of the cerebral vasculature develop such that blood flows directly from the arterial system to the venous system without passing through a capillary system. The arteriovenous (AV) shunt is the definitive characteristic of these lesions.
Frequency:
Estimated incidence of AVM in the US general population is 0.14% (140 cases per 100,000 persons or 1 case per 700 persons). This is approximately one fifth to one seventh the incidence of intracranial aneurysms.
Pathophysiology:
The direct connection between the arterial and venous systems supplies a low-resistance shunt for arterial blood and exposes the venous system to abnormally high pressures. This results in a system of enlarged feeding vessels, the tangled nidus of the AVM itself, and enlarged draining venous structures.
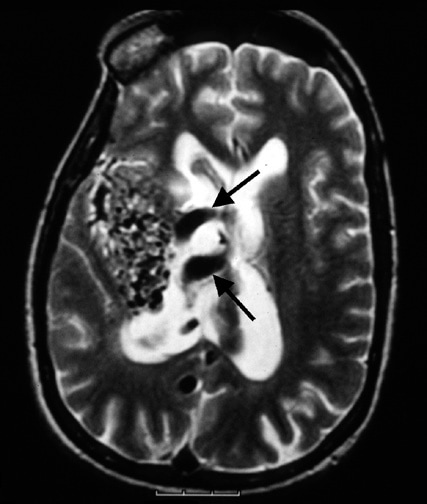
axial T2-weighted MRI shows arteriovenous malformation nidus on the right side. The arrows demonstrate large draining veins within the right lateral ventricle.
Clinical presentation:
· Hemorrhage (53% of cases)
o Acute onset of severe headache
o May be described as the worst headache of the patient’s life
o Depending on the location of hemorrhage, may be associated with new fixed neurologic deficit
· Seizure (46%)
· Headache (34%)
· Progressive neurologic deficit (21%)
o May be caused by mass effect or ischemia resulting from local vascular steal phenomenon
o Presence and nature of deficit depend on location of lesion
· Pediatric patients
o Heart failure
o Macrocephaly
o Prominent scalp veins
Hemorrhage is more likely to be caused by small lesions, while seizures are more likely to be caused by large lesions.
An increasing number of lesions now are found incidentally upon brain imaging.
The annual risk of intracranial hemorrhages associated with AVMs is 2-3%. The mortality rate associated with the initial bleed is 10%. The mortality rate associated with the second bleed is 13%, and the rate increases to 20% for each subsequent bleed. The incidence of new neurologic deficit occurring with each bleed is 50%. These numbers are generalized for all AVMs. The location and size of each patient’s lesion greatly affects their risk of morbidity and mortality.
Patients with an AVM have an increased risk of developing a cerebral aneurysm. Approximately 7.6% of patients with an AVM develop an aneurysm. Most commonly, aneurysms are found on arteries feeding the AVM.
AVMs may present as part of a neurocutaneous syndrome, including Sturge-Weber syndrome or Rendu-Osler-Weber syndrome.
Imaging studies:
· CT scan is the first imaging choice in an emergent setting in which a patient is thought to have an intracranial bleed.
· MRI is the first imaging choice in a nonemergency setting (eg, workup of seizure, headache, or neurologic deficit). Magnetic resonance angiograms (MRAs) can reveal the anatomy of the AVM noninvasively but have lower resolution than conventional angiography.
· Cerebral angiography provides definitive diagnosis.
Treatment
· Surgery
· Neurointerventional radiology
· Stereotactic radiosurgery
Comments
Post a Comment